Table of Contents
What is warfarin?
Warfarin is a synthetic derivative of coumarin, a chemical found naturally in many plants, notably woodruff (Galium odoratum, Rubiaceae)
Mechanism Of Action – Coumadin (crystalline warfarin sodium) and Warfarin are anticoagulants which act by inhibiting vitamin K-dependent coagulation factors.
More Details – Inhibits vitamin K epoxide reductase, an enzyme that recycles oxidated vitamin K to its reduced form after it has participated in the carboxylation of several blood coagulation proteins, mainly prothrombin and factor VII.
For this reason, drugs in this class are also referred to as vitamin K antagonists. Thus, warfarin indirectly prevents the synthesis of prothrombin by blocking vitamin K’s effects on prothrombin synthesis.
Normally prothrombin is converted into thrombin by Factor X (activated by thromboplastin). In turn, thrombin converts fibrionogen into fibrin forming clots.
Warfarin is the most widely prescribed anticoagulant drug in North America.
How warfarin is Clinically Applied
Used to prevent thrombosis and embolism in many disorders (some examples):
- Prophylaxis and/or treatment of venous thrombosis and its extension, and pulmonary embolism
- Prophylaxis and/or treatment of the thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement.
- To reduce the risk of death due to recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction
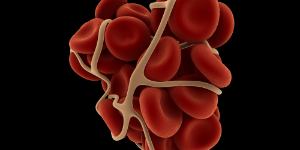
Understanding Coagulation: Coagulation begins almost instantly after an injury to the blood vessel has damaged the endothelium. Platelets immediately form a plug at the site of injury; this is called primary hemostasis.
Secondary hemostasis occurs simultaneously: Proteins in the blood plasma, called coagulation factors or clotting factors, respond in a complex cascade to form fibrin strands, which strengthen the platelet plug.
What is Thrombin?
Thrombin (activated Factor II [IIa]) is a coagulation protein that has many effects in the coagulation cascade. It converts soluble fibrinogen into insoluble strands of fibrin, as well as catalyzing many other coagulation-related reactions.
Thrombin converts fibrinogen to an active form that assembles into fibrin. Thrombin also activates factor XI, factor V, and factor VIII. This positive feedback accelerates the production of thrombin.
Factor XIII is also activated by thrombin. Factor XIIIa catalyzes the formation of covalent bonds between lysine and glutamine residues in fibrin. The covalent bonds increase the stability of the fibrin clot.
In addition to its activity in the coagulation cascades, thrombin also promotes platelet activation, via activation of protease-activated receptors on the platelet.
Why Prothrombin Time Or INR is required?
The prothrombin time (PT) and its derived measures of prothrombin ratio (PR) and international normalized ratio (INR) are measures of the extrinsic pathway of coagulation. They are used to determine the clotting tendency of blood, in the measure of warfarin dosage, liver damage, and vitamin K status.
The reference range for prothrombin time is usually around 12–15 seconds; the normal range for the INR is 0.8–1.2.
A high INR level such as INR=5 indicates that there is a high chance of bleeding, whereas if the INR=0.5 then there is a high chance of having a clot.
Normal range for a healthy person is 0.9–1.3, and for people on warfarin therapy, 2.0–3.0, although the target INR may be higher in particular situations, such as mechanical heart valves.
Are there Interactions and Dosing Problems?
Dosing of warfarin is complicated by the fact that it is known to interact with many commonly-used medications and even with chemicals that may be present in certain foods.
In order to optimize the therapeutic effect without risking dangerous side effects such as bleeding, close monitoring of the degree of anticoagulation is required by blood testing (INR).
During the initial stage of treatment, checking may be required daily; intervals between tests can be lengthened if the patient manages stable therapeutic INR levels on an unchanged warfarin dose
Major Adverse Side Effect – Fatal or nonfatal hemorrhage from any tissue or organ. Therefore, must be careful what supplements and dietary advice you give an individual on these medications.
Drug-Nutrient Interactions -Specific botanicals reported to affect coumadin therapy include the following:
- Potentiating Supplements – Bromelains, danshen, dong quai (Angelica sinensis), garlic, Ginkgo biloba, ginseng, and cranberry products are associated most often with an increase in the effects of coumadin.
- Red clover and licorice root also contain coumarins. Curcumin may also act as an anti-coagulant, as well as ginger. Omega-3 fats also act as blood thinners via their effects on PG-3 synthesis.
- Inhibiting Supplements – Coenzyme Q10 and St. John’s wort are associated most often with a decrease in the effects of coumadin.
The most dangerous herbs, which should not be taken with Coumadin, Warfarin or any anti-coagulants, including aspirin (NSAIDS) include:
- Garlic
- Ginkgo biloba
- St John’s Wort
In the case of all other supplements it is important for the patient to have their INR monitored to evaluate their effects on blood clotting and required warfarin dosage (which may require adjusting). For example, the use of omega-3 fats may reduce the required dosage of warfarin.
How Lifestyle Impacts Blood Clotting Behaviour
Increase platelet stickiness and tendency towards increased abnormal clotting behaviour is associated with:
- Overweight
- High Saturated fat diet (and cholesterol, transfats and fried foods), especially Factor VII, which ultimately increases fibrin formation – the main component of blood clots.
- Decreased aerobic fitness
- Cigarette smoking
High-Fat Meal May Raise Risk Of Blood Clotting — Increasing Heart Attack And Stroke Risk
Lone Frost Larsen (Arteriosclerosis 1997)
Plasma FVIIa increased from 48.4 units per liter (U/L) to 81.4 U/L after the high-fat meal and FVIIc increased from a mean fasting value of .81 international units (IU) to .84 IU after the high-fat meal but decreased to .72 IU among individuals following consuming the low-fat meal.
Normally when Factor VII is activated, there is an increase in fibrin, the main component of a blood clot, explains Larsen. “It starts a cascade and eventually a clot is formed. This could later block a vessel and cause a heart attack (or stroke).”
“People with heart disease already have higher levels of Factor VII,” she says. “When they have a fatty meal, Factor VII may rise even higher than in the young healthy men, which might put them at even higher risk.”
Plavix (Clopidogrel)
Mechanism Of Action – Clopidogrel is a pro-drug thought to block an adenosine diphosphate (ADP) receptor on the platelet cell membranes, known as P2Y12, which is important in platelet aggregation and cross-linking of platelets by fibrin.
More Details – The blockade of this receptor inhibits platelet aggregation by blocking activation of the glycoprotein IIb/IIIa pathway. The IIb/IIIa complex functions as a receptor mainly for fibrinogen and vitronectin but also for fibronectin and von Willebrand factor.
Activation of this receptor complex is the “final common pathway” for platelet aggregation, and is important in platelet aggregation, the cross-linking of platelets by fibrin.
Platelet inhibition can be demonstrated two hours after a single dose of oral clopidogrel, but the onset of action is slow, so that a loading-dose of 300-600 mg is usually administered.
Are there any Adverse Side Effects?
1. Severe neutropenia (Incidence: 1/2,000)
2. Thrombotic thrombocytopenic purpura (TTP) (Incidence: 4/1,000,000 patients treated)
3. Hemorrhage – The incidence of hemorrhage may be increased by the co-administration of aspirin
- Gastrointestinal Hemorrhage (Incidence: 2.0%)
- Cerebral Hemorrhage (Incidence: 0.1 to 0.4%)
- Use of non-steroidal anti-inflammatory drugs is discouraged in those taking clopidogrel due to increased risk of digestive tract hemorrhage
Plavix has been the 2nd top selling drug in the world in recent years and was still growing by over 20% in 2007. In 2005 it had sales of US$5.9 billion.

